Coproducing medical student training
22 August 2023
At the end of 2022, in collaboration with Dr Kate Pitt from Arch Healthcare, Brighton and Hove Common Ambition (BHCA) co-produced a new Student Selected Component (SSC) called Homelessness and Health. It was delivered in January 2023 to ten students at Brighton and Sussex Medical School.
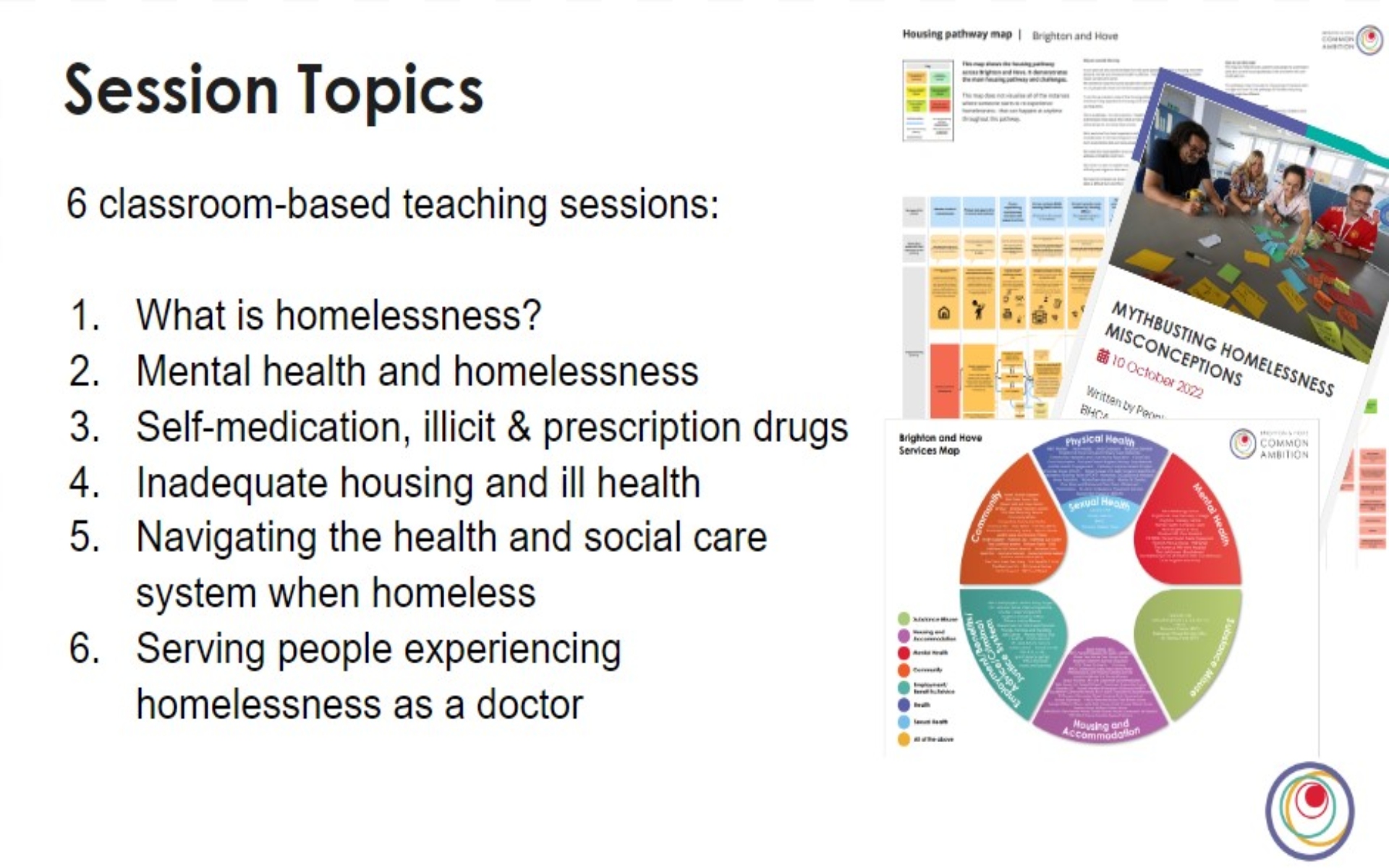
Over 5 workshops, the Common Ambition Steering Group and Kate worked together to co-design the course structure, content and teaching style. Pre-existing Common Ambition resources were used, for example blogs, service maps and housing pathway maps.
There were six teaching sessions including topics like: ‘What is homelessness?’ and ‘Mental health and Homelessness’. Each session contained a BHCA key message which often challenged outdated views and definitions of homelessness.
The module also included a session where BHCA members and students met to discuss and reflect on the course and its issues raised together. This worked really well; everyone felt safe and welcome.
We wanted to encourage critical thinking and reflective practice which we feel was achieved. This was done by ensuring lots of discussion in sessions, leaving space to check in and out, and providing lots of opportunities to feedback and ask questions.
The feedback from the students was fantastic, with all students saying they enjoyed the course, some arguing it should be mandatory, and others valuing the time and space for discussion and reflection. The course was oversubscribed, and was so successful it has been approved to run every term from October 2023!
We considered one point of feedback in more detail which was “it would be good if a patient would like to come in and share with us what they’d like from us as future doctors and their own experiences and views that don’t mind being asked some questions.” Because we work in a trauma-informed way, we try to avoid sharing personal stories which can be triggering to share and hear. We feel the following questions should be well thought out before using patient stories of experience teaching:
- How will sharing stories and experiences feel for the patient?
- What is the value and purpose of ‘lived experience’ stories?
- Can my work be done without someone sharing their personal challenging experiences?
- How can I ensure I am working collaboratively and ‘alongside’ a patient in this setting?
- Do I have consent to share someone’s story/experience?
There was lots of learning from this process and after feedback and discussions with students, we will be making improvements to the Student Select Component for the next time it runs.
We believe this work impacts future doctors, especially around incorporating a holistic approach to supporting people. We are grateful for the opportunity to share what we have learnt from our lived experience and be listened to. It proved co-production works for everyone involved. We believe co-production and patient participation should be incorporated into all doctor training and service design because it is so valuable – To quote one of a group member “you won’t be able to see what we can see”.
Dr Kate found the experience eye-opening and gained a lot from the work. Firstly, BHCA highlighted that ‘“‘Official’ definitions and models are flawed and need to be critiqued.” Kate also learnt that effective co-production needs time and investment. Finally, the work showed Kate that different perspectives bring richness to teaching and most importantly that “we learn most from the people we serve”.
A note from Inessa Alekseeva, a medical student who undertook the SSC:
Homelessness and Health SSC Feedback:
This was an amazing SSC that really opened my eyes to the challenges people experiencing homelessness face and the different barriers to care they come across. One of the best parts of the SSC was the opportunity to direct questions to people with lived experiences of homelessness. It was truly a privilege to do this, and the answers were very valuable for us to understand their perspective on different issues.
While we all acknowledge that being homeless is extremely hard, I only now realise just how unfair and discriminating the system is towards this group of people. The wide range of topics we explored in our sessions allowed me to get a bigger picture of the issues surrounding homelessness. It was appalling to see the statistics on the wide range of health issues this population faces with almost no support. The vicious cycle between poor mental health and substance misuse was something I had never really thought about before this training. It was shocking to find out that half of the homeless population experienced abuse and traumatic events in their childhood, with even more experiencing it while being homeless every day. It is not surprising that many turn to alcohol and drugs as coping mechanisms. Getting help is extremely hard for anyone with a mental health issue, but it is ten times harder for people sleeping rough. Not only the practical part of it is very complicated and requires immense effort, but the distrust in the doctor-patient relationship and the fear of being constantly doubted and stigmatised are all very valid reasons why some choose not to engage with health services.
I strongly believe this SSC should be a part of every healthcare practitioner’s training, especially doctors. Any doctor would encounter a person experiencing homelessness at least once in their career. Therefore, it is crucial we understand the difficult circumstances that push people into homelessness and the challenges of sleeping rough to deliver the best care possible. The SSC made me realise how creating a safe and trusting environment, being patient, and understanding the full picture of an individual’s life are all key in caring for the homeless.
If you have any questions on this work or wish to discuss how we can collaborate on something similar, do get in touch with Nicky Pyper, Project Manager.